Introduction
Over the past several years, MDMA (also known as Ecstasy/Molly) has been making waves in the realms of drug research and therapy, with many efforts having been largely spearheaded by MAPS. Recognized for its ability to enhance feelings of empathy and bonding among users, research has largely aimed at examining MDMA’s therapeutic potential for those dealing with various emotional burdens such as trauma (Sessa, Higbed, & Nutt, 2019).
The history of the drug, although complex, can be broadly examined through its discovery, early testing and therapeutic uses, prohibition, and resurgence.
History
In their article, The History of MDMA as an Underground Drug in the United States, 1960-1979, Passie and Benzenhöfer (2016) offer a glimpse into the discovery and early testing of MDMA. Merck, a German pharmaceutical company, first synthesized MDMA in 1912 while in pursuit of a life-saving medicine that would help blood to clot; the drug was then patented in 1914 (Passie & Benzenhöfer, 2016). The authors note that between the years of 1927 and 1959, animal testing was conducted several times at Merck and within U.S. army laboratories but the findings were not publicly disclosed.
The effects of MDMA in humans were not explored until the 1970s (Passie & Benzenhöfer, 2016). Following the ban of lysergic acid diethylamide (LSD) in the 1960s, US-based psychotherapists sought alternative methods of healing (Sessa, Higbed, & Nutt, 2019). Upon being introduced to MDMA through chemist Alexander Shulgin, psychotherapist Leo Zeff went on to administer thousands of doses to patients and Shulgin subsequently published the first report of the effects of the drug in humans (Sessa, Higbed, & Nutt, 2019; Shulgin, 1978). Unfortunately, research did not progress much farther past this point, as prohibitory measures began closing in.
During the 1960s, MDMA’s presence in the underground drug scene was on the rise in the US. Small-scale distribution efforts grew larger through the 1970s and early 1980s, resulting in its eventual prohibition in 1985 (Sessa, Higbed, & Nutt, 2019). Passie and Benzenhöfer (2016) draw attention to similarities in the Canadian context where, as a consequence of illegal production and market sales through the 1970s, the drug was scheduled in 1976. This meant years of research progress had come to a sudden halt, with MDMA’s pharmacological properties and therapeutic potential left vastly unexplored. However, studies published prior to prohibition were useful in furthering our understanding of the pharmacological properties of MDMA.
The Pharmacology of MDMA
To understand MDMAs action, we must understand its pharmacology, in particular its modes, uses and effects. 3,4-MethyleneDioxyMethAmphetamine (MDMA) is a chemical molecule that, upon oral ingestion, is absorbed by the blood and carried to the brain, where it produces its psychoactive effects. Most often found in the form of tablets, typical doses for recreational use range from 50 to 150mg. The pharmacology of MDMA can be understood as a sequential process.
- After ingestion, the molecule travels through the gastrointestinal tract and gets absorbed over the course of 2 hours. The psychological effects kick in 30-60 minutes after administration, as this is the time it takes for the molecules to reach the brain.
- In the brain, MDMA has to cross the blood-brain barrier (this protects the brain from toxins and allows nutrients to pass through). How it crosses the barrier is not completely understood, but some studies compared its mode of passing with other amphetamines, and these amphetamine-like qualities seem to be responsible for most of the undesired effects (Kousik, Napier, & Carvey, 2012).
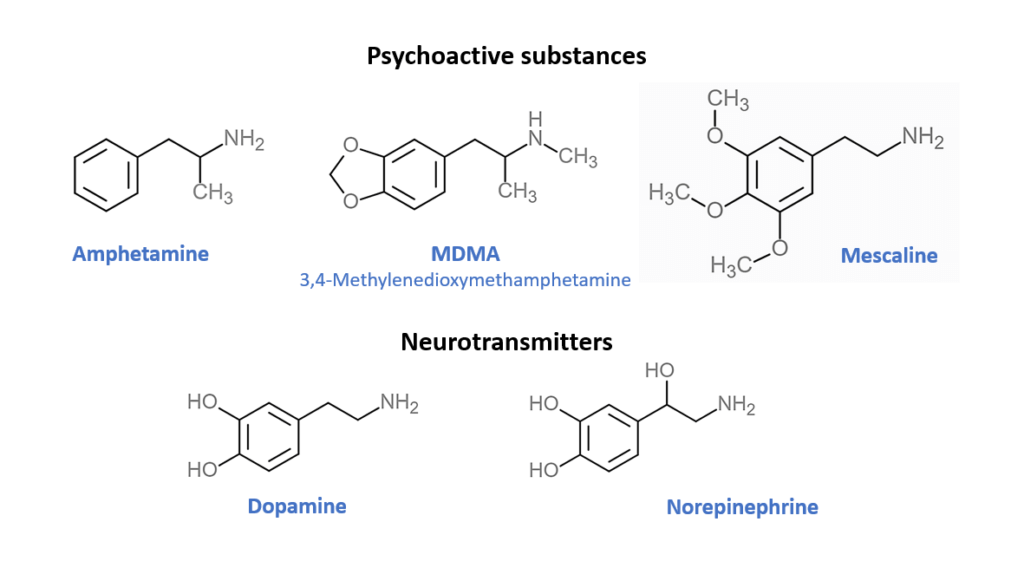
- After crossing the barrier, MDMA binds to several different types of receptors in the brain. The lock and key analogy illustrates this concept quite well. MDMA mimics the shape of natural neurotransmitters (neurotransmitters are molecules by which the neurons communicate with each other) in particular serotonin, dopamine, and noradrenalin. Serotonin is considered to be responsible for mood, depression and feeling of well-being, dopamine on the other hand responsible for pleasure and motivation. So it acts as a key for several different locks (receptors), it increases the concentrations of the keys (neurotransmitters), so with more of them more locks (receptors) can be activated. However, the receptors are not located everywhere but each of them have their specific region in the brain. The unique effect of MDMA is due to the combination of receptors and neurotransmitters that produce a unique pattern of brain activity which is responsible for the psychological effects of MDMA including increases in well-being and sociability, extraversion, a heightened sense of closeness and a greater tolerance of other views.
- However, MDMA is considered to have some distinct effects compared to standard psychedelic drugs , such as psilocybin or LSD. The distinction lies in their chemical structure. Compare for yourself the similarities with classic psychedelics (mescaline) and amphetamine, and their overall resemblance with neurotransmitters in your brain (see the illustration). This combined effect of the amphetamine-like structure and mescaline/LSD-like structure affect the dopamine system, while producing physical effects (such as wakefulness, endurance and sense of energy, postponed fatigue/sleepiness), and the serotonin system that produces psychoactive effects psychedelics are mostly known for. This combination of two neurotransmitter systems produces MDMA’s unique psychological qualities.
- We should not forget about the unique effect of MDMA on oxytocin, also called “love hormone”, since it is the hormone that is implicated in romantic love, and was found to spike during the honeymoon phase of relationships (Schneiderman, 2012). But it also has effects on lowering anxiety, increasing pair bonding (long term commitment) and facilitating pro social behaviors (Holze, Vizeli, Müller, et al., 2020). Unfortunately the mechanisms by which MDMA engages oxytocin need more research.
- Kalant (2001) outlines that even though the liver starts breaking down MDMA in your bloodstream immediately upon absorption, it takes around 8 hours to break down 50% of the substance. Additionally, the molecules that degrade MDMA in the liver are limited, so the body is very sensitive to the administration of high doses that greatly surpass liver breakdown capabilities (Kalant, 2001). Most of the MDMA tablets that are produced illegally have variable concentrations of the MDMA compound in them, varying 70-fold or more (Kalant, 2001). This variability can pose serious risks and induce neurotoxicity at high concentrations, meaning controlled production and regulations are needed to objectively assess the risks and benefits of MDMA.
Conclusion
In 2010, researchers at MAPS USA published, The safety and efficacy of ±3,4-methylenedioxymethamphetamine-assisted psychotherapy in subjects with chronic, treatment-resistant posttraumatic stress disorder: the first randomized controlled pilot study, The study re-launched a long-forgotten field of scientific inquiry, setting the stage for subsequent research efforts that brought us the knowledge we have today. In recent years, MAPS has published several more studies examining the effects and potential therapeutic benefits of MDMA.
References
Holze, F., Vizeli, P., Müller, F., Ley, L., Duerig, R., Varghese, N., Eckert, A., Borgwardt, S., & Liechti, M. E. (2020). Distinct acute effects of LSD, MDMA, and D-amphetamine in healthy subjects. Neuropsychopharmacology, 45, 462–471. https://doi.org/10.1038/s41386-019-0569-3
Kalant, H. (2001). The pharmacology and toxicology of “ecstasy” (MDMA) and related drugs. Canadian Medical Association Journal, 165(7), 917-928.
Kousik, S. M., Napier, T. C., & Carvey, P. M. (2012). The effects of psychostimulant drugs on blood brain barrier function and neuroinflammation. Frontiers in Pharmacology, 3, 121. https://doi.org/10.3389/fphar.2012.00121
Mithoefer, M. C., Wagner, M. T., Mithoefer, A. T., Jerome, L., & Doblin, R. (2010). The safety and efficacy of ±3,4-methylenedioxymethamphetamine-assisted psychotherapy in subjects with chronic, treatment-resistant posttraumatic stress disorder: the first randomized controlled pilot study. Journal of Psychopharmacology, 25(4), 439–452. https://doi.org/10.1177/0269881110378371
Passie, T., & Benzenhöfer, U. (2016). The history of MDMA as an underground drug in the United States, 1960–1979. Journal of Psychoactive Drugs, 48(2), 67-75. https://doi.org/10.1080/02791072.2015.1128580
Schneiderman I, Zagoory-Sharon O, Leckman JF, Feldman R. Oxytocin during the initial stages of romantic attachment: relations to couples’ interactive reciprocity. Psychoneuroendocrinology. 2012;37(8):1277-1285. doi:10.1016/j.psyneuen.2011.12.021
Sessa, B., Higbed, L., & Nutt, D. (2019). A review of 3,4-methylenedioxymethamphetamine (MDMA)-assisted psychotherapy. Frontiers in Psychiatry, 10, 138. https://doi.org/10.3389/fpsyt.2019.00138
Shulgin, A. T., & Nichols D. E. (1978). Characterization of three new psychotomimetics. In: Stillman, R.C., & Willette, R.E. (Eds). The Psychopharmacology of Hallucinogens. New York, NY: Pergamon Press.
Rubio-Araiz, A., Perez-Hernandez, M., Urrutia, A., Porcu, F., Borcel, E., Gutierrez-Lopez, M. D., O’Shea, E., & Colado, M. I. (2014). 3,4-methylenedioxymethamphetamine (MDMA, Ecstasy) disrupts blood-brain barrier integrity through a mechanism involving P2X7 receptors. The International Journal of Neuropsychopharmacology, 17(8), 1243–1255.